A Pandemic Resilient World

Contagious diseases are a fact of human life. Quite often, they are also a cause of death.
All living organisms are continuously exposed to a plethora of viruses and microorganisms (such as bacteria). Most of these are harmless to humans, and some are beneficial, but a small number can infect us and potentially make us very ill (or even kill us).
If all the 1 × 1031 viruses on earth were laid end to end, they would stretch for 100 million light years. There are 100 million times as many bacteria in the oceans (13 × 1028) as there are stars in the known universe.
Most viruses (and other pathogens) are native to a specific species. Over time the host organism will acquire some degree of immunity against the pathogen, minimizing the consequences of infection and limiting its transmissibility.
Occasionally, a combination of random genetic mutations and bad luck will allow a pathogen to cross the “host range barrier” and infect a new host species. Without the same degree of acquired immunity, the new host can become very ill and rapidly spread the infection. All of the most severe pandemics in human history started as outbreaks when a virus (or bacteria) lept from an animal “reservoir” of infection to a human host.
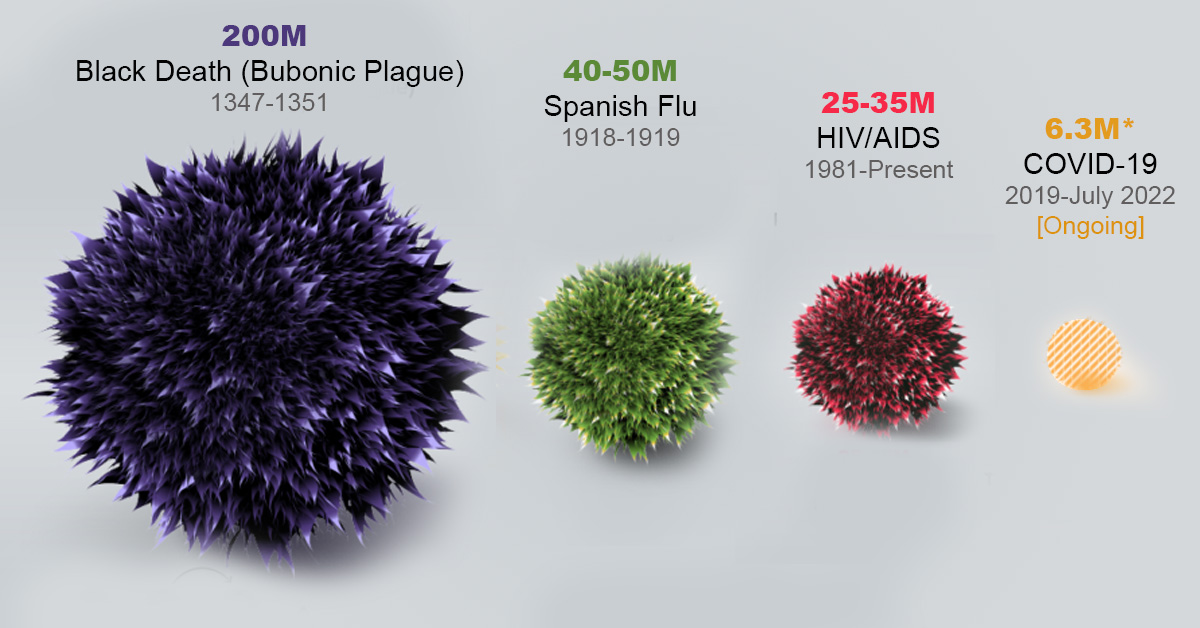
The results can be disastrous. In 1918 the H1N1, endemic in pigs, spread to humans and ended up killing more than twice as many people as in the First World War. That was the bloodiest conflict in human history and coincidentally ended the same year. In the Middle Ages, the Black Death killed up to 200 million people including half of the European population. It was caused by a bacterial infection that jumped to humans from rats via fleas.
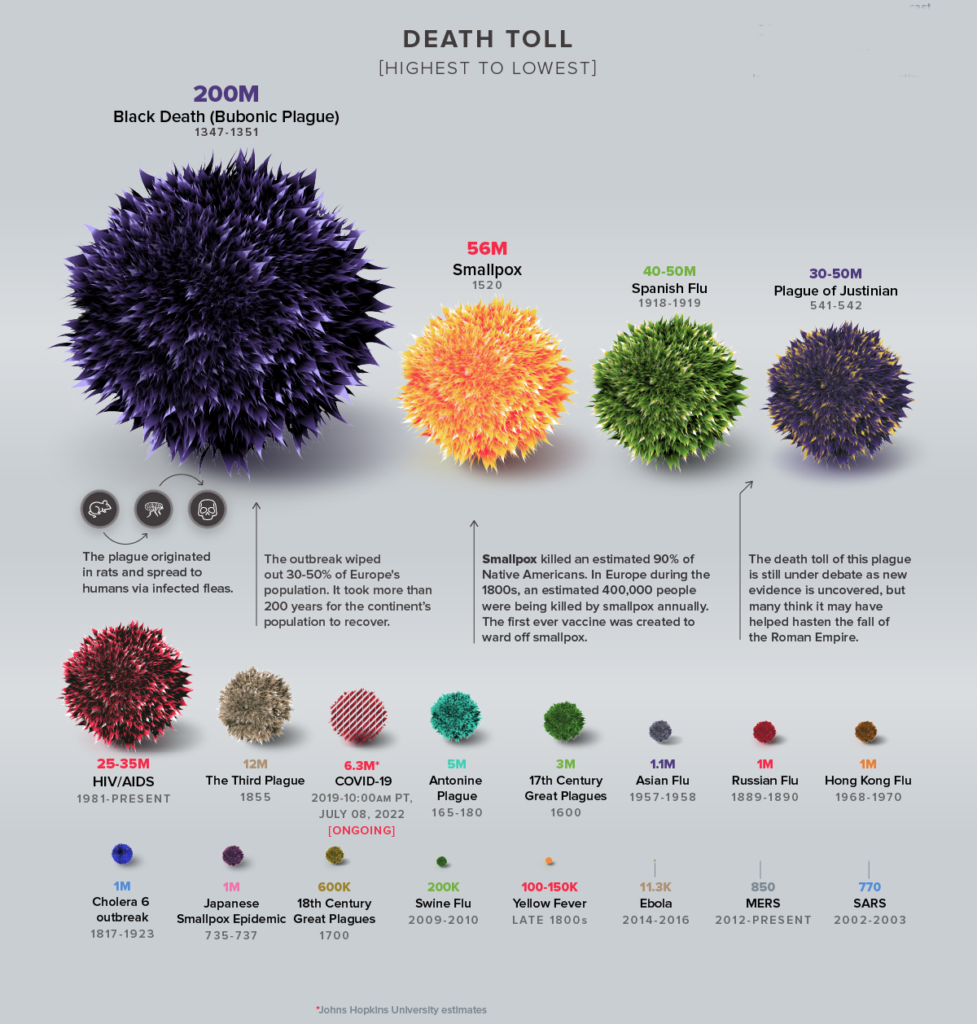
On this scale, the Covid-19 pandemic (probably caused by the SARS-CoV-2 virus jumping from a bat to a human host), wasn’t particularly serious, despite causing millions of deaths and trillions of dollars of lasting economic damage. Neither was it particularly surprising. After the near misses of the SARS, MERS and Ebola outbreaks, World Governments, despite their apparent unpreparedness, have been expecting a pandemic for a while.
Outbreaks are inevitable, but pandemics are optional.
Dr Larry Brilliant, epidimeologist.
In an overpopulated, highly interconnected, and predominantly urban world, it’s only a matter of time before the next outbreak of a novel contagious disease. While we can’t prevent these outbreaks, we can minimize their impact. In this article, we explore four ways in which simulation is making the world more resilient to future pandemics.
1. Reducing infection rates
In the early days of an epidemic, when the immunity of a population is low, the greatest challenge for public health institutions is controlling the rate of infection.
The rate of spread of infectious disease into a population is defined by a parameter called the Reproduction Number (often called the “R Number”), which represents the average number of secondary infections caused by each infected person. If R is consistently less than one, the epidemic is in decline. An R number much greater than one indicates that the disease is spreading exponentially.
Typically airborne viruses have a much higher R number than pathogens that require physical contact or the exchange of bodily fluids. For example, measles (spread by sneezing) is among the most contagious diseases and has an R number of between 12 and 18. Ebola (spread through bodily fluids) has an R number of between 2 and 3. The Omicron variant of the Covid-19 virus had an R number of about 9, meaning that each infected person could expect to spread the disease to 9 other people.
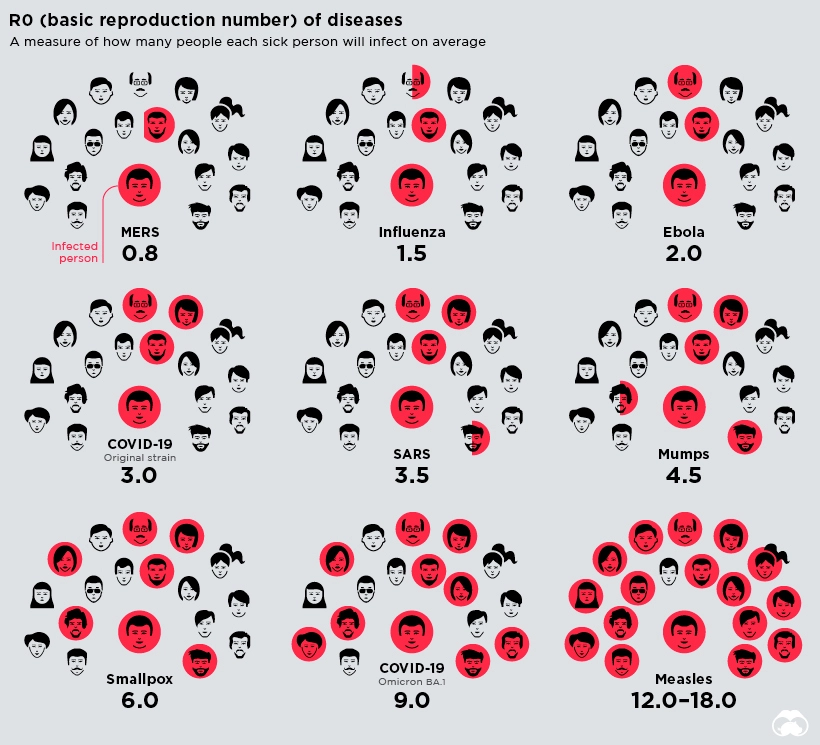
Although they can’t directly affect how infectious the pathogen is, governments can introduce a variety of public health interventions to try and reduce the spread of the infection. Here simulation plays a key role in understanding modes of transmission and how they can be mitigated:
- One of the most controversial interventions in the Covid-19 pandemic was compulsory mask-wearing. Many argued that the poorly fitted masks did little to protect against the transmission of the virus through airborne mucus particles from coughs and sneezes. Simcenter helped to demonstrate the efficacy of face coverings and to illustrate the deficiency of poorly fitted masks.
- Jaros, Baum & Bolles, an engineering consulting firm, worked closely with the New York Times to show how schools can reduce COVID-19 exposure in classrooms by opening windows. The engineers at JB&B used Simcenter CFD simulations to show how contaminants from an infected student circulate in a classroom.
- Siemens and Airbus used Simcenter to understand the transport of particles/droplets from a human cough in an aircraft cabin. Using CFD simulations, the team has modeled the transport of cough droplets in an aircraft cabin.
- UES, Inc. partnered with the US Air Force Research Laboratory’s 711th Human Performance Wing (HPW) and used Simcenter to simulate a cough from an infected passenger in a C-130 Hercules aircraft with multiple passengers. The CFD simulations’ results helped improve procedures and sampling strategies for bioaerosol detection and surface decontamination.
- Using CFD simulation with Simcenter, the engineers at Norton Straw analyzed the airflow in a train cabin resulting from many mitigation strategies – windows open, a plastic shield between passengers, different ventilation airflow, etc.
Of course, public health interventions can only do so much to reduce the transmission of particularly virulent infectious diseases. The only real hope of ending any epidemic is through accumulated herd immunity.
In order to control the rate of infection, then public health agencies need to be able to accurately measure the rate of infection across a population. They also need to quickly and reliably identify infected individuals so that they can be quarantined to prevent further infections.
One of the worst failures [of the Covid pandemic] is that the United States never got testing right. Not nearly enough people were tested and results took far too long to come back. If you’re carrying a virus but don’t know it for another seven days, you’ve just spent a week potentially infecting other people.
Bill Gates, How to Prevent the Next Pandemic
During the Covid pandemic, legitimate concerns arose about the accuracy of testing, especially of rapid testing devices used by patients to test themselves at home. This led to a great deal of re-engineering behind the scenes, often led by simulation, and to the evolution of rapid testing devices as the pandemic progressed.
2. Faster vaccine production
Vaccines trick the immune system into “recognising” a virus that it has never been exposed to. By providing it with a “preview” of the virus structure, vaccines allow the patient’s immune system to design potent antibodies that neutralise the actual virus if the individual is ever infected. The World Health Organisation estimates that 2-3 million lives a year are saved as a result of vaccination.
Unfortunately, traditional vaccines – which work by exposing the patient to a weakened or inactivated strain of the virus – can take years (or even decades) to develop and gain regulatory approval, which is no good in combatting a fast-moving novel pandemic.
During the Covid-19 pandemic, world governments rushed through regulatory approval of RNA and DNA vaccines. These vaccines work by injecting a portion of the virus’ genome into the patient.
Once absorbed by host cells, these genetic instructions tell the cell to manufacture multiple copies of specific virus proteins (usually spike proteins) for several days. The synthetic genetic material is only a partial copy of the genome that cannot replicate. Still, it is enough to train the patient’s immune system to develop antibodies to attack the virus.
The challenge is that these strands of genetic material are fragile and need to be protected on their journey into the cells of the patient.
- For synthetic mRNA vaccines (such as Pfizer-BioNTech and Moderna), the genetic material is encased within a bubble of lipid nanoparticles. The diameter of each is measured in tens of nanometers (there are a million nanometers in a single millimetre). Because of the scale of the particles involved and the fragility of the RNA, macroscale bulk mixing is not effective. The whole field of microfluidics depends entirely on multiphase computational fluid dynamics simulations to design and validate the devices, and synthetic vaccine production would not be impossible without digital simulation.
- Viral vector vaccines (such as the one from Oxford-AstraZeneca) use a genetically engineered adenovirus (a common cold-like virus) to carry DNA into host cells. These “virus infected” cells are grown inside bioreactors, literally virus farms, carefully controlled nutrient enriched mixing environments in which the temperature, oxygen and pH are precisely controlled to maximize the yield of both the cells and viruses. biological processes do not scale linearly with the geometric size of the bioreactor. Maintaining the ideal cultivation conditions developed in a 10-litre bench experiment in a 4000-litre industrial bioreactor is a complex engineering problem, which is again highly dependent on computational fluid dynamics.
Siemens helped BioNTech convert a facility in Marburg, Germany, to produce its mRNA COVID-19 vaccine, which it developed with Pfizer, in record time: cutting the estimated over-a-year timeline to just five months with automation and digitalization technology.
You can read more about the role the Simcenter played in vaccine production for the Covid-19 pandemic by reading “Digital Vaccines for Digital Viruses”.
3. Better vaccine delivery
Once an effective vaccine is available, the next challenge is implementing an effective delivery program. The problem here is that administering vaccines requires a degree of medical training. One of the struggles of the COVID-19 pandemic was mobilizing enough trained medical professionals to administer the vaccines. This included bringing many doctors and nurses out of retirement. Another issue was manufacturing enough active vaccines required to administer more than 12 billion doses worldwide.
Siemens’ customer Voxdale is using Simcenter to design an automated intradermal vaccination device that could solve these problems for future pandemics. Intradermal means ‘into the skin’ instead of intermuscular, which means ‘into the muscle’.
The advantage of injecting into the skin is that it takes only 1/10th of the vaccine required to have the same effect as an intermuscular injection. This is a significant saving when manufacturing, transporting and administrating tens of billions of vaccine doses.
The problem is that dermis is very thin – about 1 to 4 mm, and offers a much smaller target than injecting into muscle. So injections need to be incredibly precise. Intradermal vaccination is historically challenging to apply manually. It requires specialised training to insert a needle at an angle of 10 to 15 degrees to the skin’s surface (known as the Mantoux technique). Too shallow, and it will leak onto the surface of the skin. It has been shown that about 70% of intradermal injections using the Mantoux technique are incorrectly administered.

Once the reliability of the device has been demonstrated (and been through the arduous regulatory approval process) devices such as these offer the prospect of fully automated vaccination clinics that do not require hordes of expensively trained medical professionals to administer a simple jab.
4. Global vaccination
As successful as the Covid-19 vaccination programme was, delivery was biased towards those living in the most economically developed countries. Only 20.9% of people in low-income countries have received at least one dose. Not only is this a problem for the people that live in those countries, but it also is an issue for attempts to irradicate the virus. These unvaccinated populations provide a reservoir of infection in which the virus has a chance to mutate and evolve, possibly into a more virulent form that can re-infect vaccinated populations.
One issue is making enough vaccines for everyone, a problem discussed above. Another is finding enough medically trained people to deliver them effectively, also discussed above.
Another significant challenge is delivering temperature-sensitive vaccines to remote communities. Vaccines must be kept within a specific temperature range to avoid being spoiled.
Voxdale has used Simcenter to design a battery-powered vaccine carrier capable of maintaining the temperature of vaccine doses in a tightly specified temperature range (typically between 2 and 6C) on long road trips in hot countries.
The Covid-19 pandemic was a wake-up call that the mutation of a few genes in an animal-hosted virus can have devastating consequences in terms of lost human life, restriction of freedom and near-catastrophic economic damage. Infectious outbreaks of novel viruses are inevitable (and likely to increase in frequency). As a species, we need to be better prepared for the next one. We simply cannot afford a repeat of the death and destruction caused by a random mutation in the SARS-CoV-2 virus. While it isn’t a panacea, engineering simulation will certainly play a key role in making us resilient against the next pandemic.


